Case Study: Capturing Savings Across Claim Complexity with a Tiered Payment Integrity Strategy
How Valenz Clean Claim Verification Uncovered $43.4M in Potential Savings Across 626K Claims
Executive Summary
A large healthcare plan payer partnered with Vālenz Health® to conduct a comprehensive review of more than 626,000 medical claims incurred over six months to capture potential savings from billing inaccuracies, coding errors, and clinical discrepancies across both participating and non-participating providers.
To address the scale and complexity of the claims dataset, Valenz deployed its Clean Claim Verification solution, applying a three-tiered, severity-based review model that relies on an automated claim editing engine fueled by data curated by a certified medical coding team.
In total, the dataset represented $539 million in billed charges, reduced to $176 million in allowed charges after contractual adjustments. Using its proprietary review process, Valenz identified potential savings of $112.6 million in initial billed charges, reduced to $43.4 million in allowed charges.
Nearly three-quarters of total coding edits leading to savings were identified in the first two tiers of review, highlighting the strong return on investment achievable through automated and mid-complexity clinical reviews at scale.
Sem Ipsum
Lorem ipsum dolor sit amet consectetur adipisicing elit. Ratione hic quaerat magnam accusantium sequi inventore non quod, maiores veniam recusandae maxime repudiandae impedit, obcaecati atque, iusto molestiae repellendus veritatis commodi illo ex ab! Maxime harum est ad suscipit sint delectus.
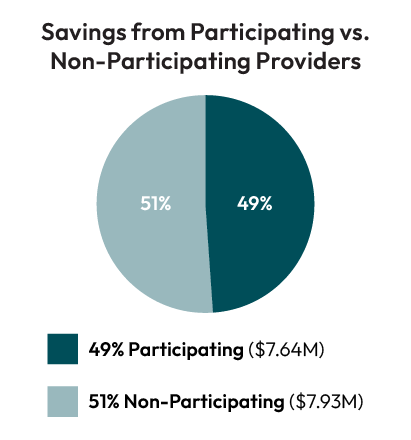
Furthermore, analysis revealed that non-participating providers contributed $28.7 million in total allowed charges across all review levels, for 66.2% of all charges for the healthcare plan payer — demonstrating a strong business case for out-of-network-specific claims review solutions.

By aligning the level of review to claim complexity, Valenz helped the payer maximize savings and improve payment accuracy at scale through comprehensive, full-cycle payment integrity solutions that outperform one-size-fits-all approaches.
Challenge:
A healthcare plan payer engaged Valenz to perform a comprehensive review of 626,413 claims incurred over six months to identify billing inaccuracies, coding errors, and clinical discrepancies across participating and non-participating providers, with the end goal of reducing the payer’s financial burden while ensuring provider payments were fair and accurate.

Fusce a quam. Curabitur vestibulum aliquam leo. In dui magna, posuere eget, vestibulum et, tempor auctor, justo. Suspendisse eu ligula. Suspendisse non nisl sit amet velit hendrerit rutrum. Praesent egestas tristique nibh. Donec posuere vulputate arcu. Vestibulum turpis sem, aliquet eget, lobortis pellentesque, rutrum eu, nisl. Praesent metus tellus, elementum eu, semper a, adipiscing nec, purus. Sed libero.
Short-term goal
Lorem ipsum dolor sit amet consectetur adipisicing elit. Ratione hic quaerat magnam accusantium sequi inventore non quod, maiores veniam recusandae maxime repudiandae impedit.
Long-term goal
Lorem ipsum dolor sit amet consectetur adipisicing elit. Ratione hic quaerat magnam accusantium sequi inventore non quod, maiores veniam recusandae maxime repudiandae impedit.
Solution:
To quickly and accurately review the large dataset of claims, we deployed the comprehensive Valenz Clean Claim Verification solution — medical coding software that scrubs and reviews all inpatient, outpatient, and specialty data for industry-leading claim editing.
Using a tiered approach, Valenz reviewed and identified savings at three levels of claim severity:
-
Highest Severity: Primary editing to capture errors in basic coding rules, duplications, and unbundling violations — in other words, those services that should never be paid due to fundamental errors
-
Medium Severity: Secondary editing, requiring medical necessity assessment, appropriate use criteria, and evidence-based guidelines — in other words, those services billed incorrectly based on specific circumstances, modifier usage, or demographics
-
Least Severity: Tertiary editing, which assess appropriateness of care, experimental/investigational determinations, and complex medical necessity disputes— in other words, those services where more appropriate coding or billing practices may apply
Results:
With this comprehensive approach to payment integrity, Valenz identified more than $43.4 million in total allowed charges across all three levels of claims and across both participating and non-participating providers.
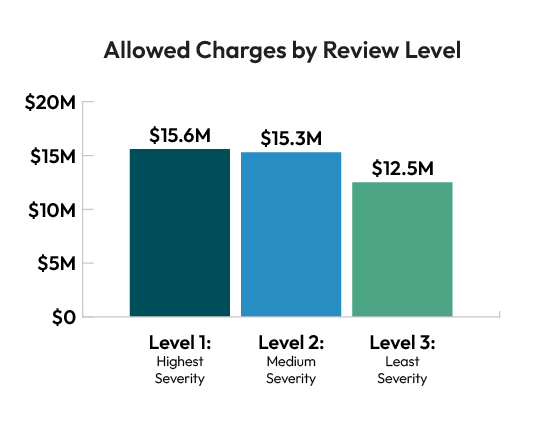
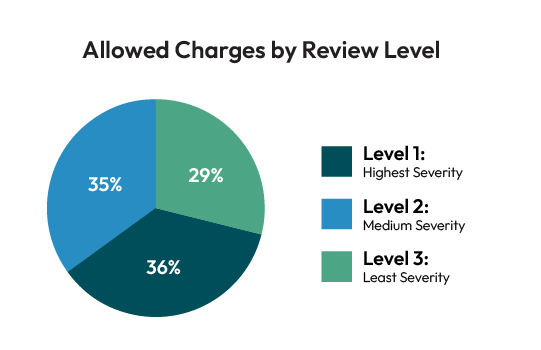
The majority of savings within allowed charges was identified in the first two tiers of complexity (Level 1 representing 35.9% and Level 2 representing 35.3% of total savings), suggesting that mid-complexity clinical validation represents the “sweet spot” for volume-based savings identification, while foundational automated edits provide substantial returns with minimal manual intervention.
Level 1: Primary Editing (35.9% of Savings)
Our foundational claims review identified $15.6 million in allowed charges out of $39.5 million in initial billed charges across this level of claims.
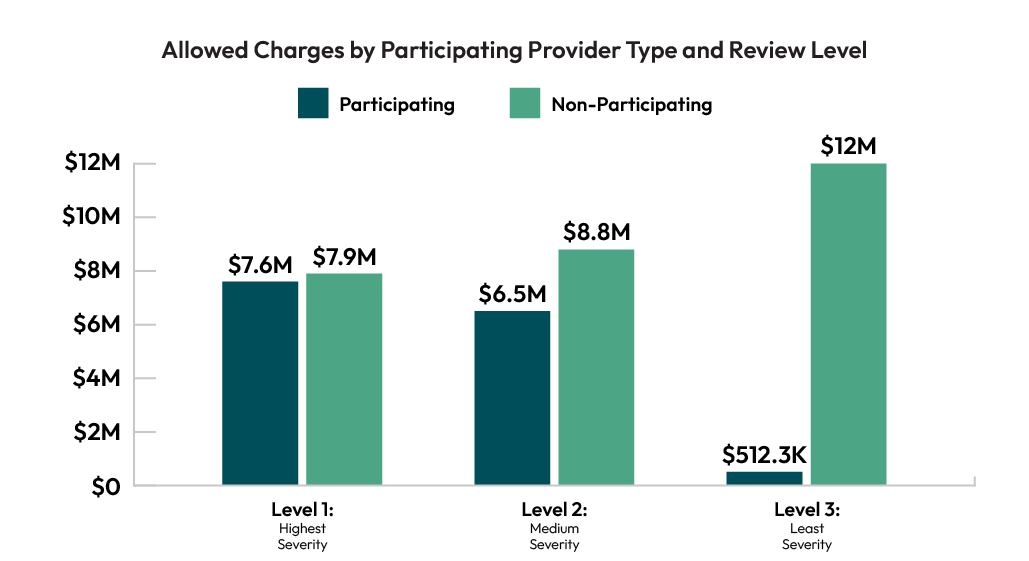
Analysis revealed that 49% of these savings came from participating providers, demonstrating that even in-network providers with established relationships can create significant billing leakage at this claim editing level.
Level 2: Secondary Editing (35.3% of Savings)
The second level of review generated the highest dollar volume of potential savings, totaling $43.6 million in initial billed charges and $15.3 million in final allowed charges, serving as the largest single contributor to the program’s overall financial impact.
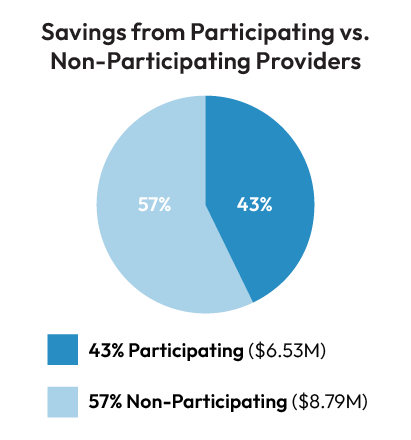
The near parity between participating (43%) and non-participating (57%) claim attribution at this level demonstrates the importance of equal review of both out-of-network and in-network claims for maximum savings identification.
Level 3: Tertiary Editing (28.9% of Savings)
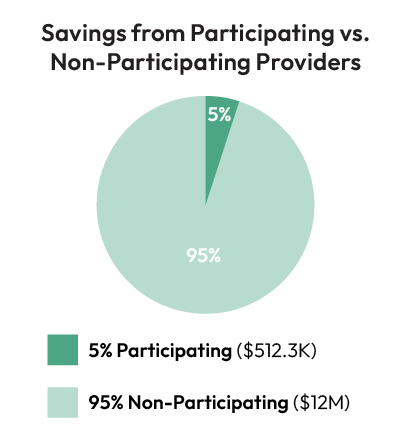
The final level of claim review identified the most dramatic provider-attribution finding of the entire claims analysis: 95.9% of allowed charges in this tier originated from non-participating providers, for a total of $12 million in potential savings.
In total, the final tier of claim review identified $29.4 million in billed charges and $12.5 million in allowed savings.
Conclusion: Capturing Savings Across Claim Complexity Comprehensive Payment Integrity Solutions
With a comprehensive, three-tiered approach to claim review, Valenz identified significant cost savings for this health plan payer, to a total tune of $43.4 million in allowed charges across a six-month period of claims with varying severity of impact.
While each tier of claims contributes measurably to overall financial incomes, the dramatic shift in provider attribution from the first to third level of severity suggests that a one-size-fits-all approach to payment integrity will underperform relative to differentiated strategies that incorporate both automated and manual claim review.
This payment integrity program demonstrates strong performance across all three levels, with clear evidence that a layered approach catches different types of billing problems — results that support investment in comprehensive, full-cycle payment integrity solutions that capture a wide variety and complexity of billed charge savings.
Lorem ipsum dolor sit amet consectetur adipisicing elit. Ratione hic quaerat magnam accusantium sequi inventore non quod, maiores veniam recusandae maxime repudiandae impedit, obcaecati atque, iusto molestiae repellendus veritatis commodi illo ex ab! Maxime harum est ad suscipit sint delectus.
Sarah Adams
Business Strategy Leader
Fusce a quam. Curabitur vestibulum aliquam leo. In dui magna, posuere eget, vestibulum et, tempor auctor, justo. Suspendisse eu ligula. Suspendisse non nisl sit amet velit hendrerit rutrum. Praesent egestas tristique nibh. Donec posuere vulputate arcu. Vestibulum turpis sem, aliquet eget, lobortis pellentesque, rutrum eu, nisl. Praesent metus tellus, elementum eu, semper a, adipiscing nec, purus. Sed libero.
Conclusion: Capturing Savings Across Claim Complexity Comprehensive Payment Integrity Solutions
With a comprehensive, three-tiered approach to claim review, Valenz identified significant cost savings for this health plan payer, to a total tune of $43.4 million in allowed charges across a six-month period of claims with varying severity of impact.
While each tier of claims contributes measurably to overall financial incomes, the dramatic shift in provider attribution from the first to third level of severity suggests that a one-size-fits-all approach to payment integrity will underperform relative to differentiated strategies that incorporate both automated and manual claim review.
This payment integrity program demonstrates strong performance across all three levels, with clear evidence that a layered approach catches different types of billing problems — results that support investment in comprehensive, full-cycle payment integrity solutions that capture a wide variety and complexity of billed charge savings.